9th Edition
World Heart Congress
THEME: "Heartbeat of Change: Inspiring Solutions for Global Cardiac Health"
 17-18 Nov 2025
17-18 Nov 2025  Dubai, UAE (Collaboration with the Armenian Cardiologists Association)
Dubai, UAE (Collaboration with the Armenian Cardiologists Association) THEME: "Heartbeat of Change: Inspiring Solutions for Global Cardiac Health"
 17-18 Nov 2025
17-18 Nov 2025  Dubai, UAE (Collaboration with the Armenian Cardiologists Association)
Dubai, UAE (Collaboration with the Armenian Cardiologists Association) 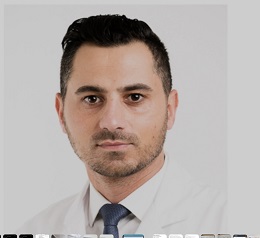
Cliniques Universitaires Saint Luc, Belgium
Title: Robotic Mitral Valve Repair: A 12-Year Experience from a Single Institution
Gaby Aphram is a Belgian cardiac surgeon at the Cliniques universitaires Saint-Luc (CUSL) in Brussels. He graduated from UCLouvain in 2011 and completed his cardiac surgery training in Belgium and Strasbourg, earning his specialist qualification in 2017. After a fellowship in valvular surgery under Prof. Gébrine El Khoury and advanced training in percutaneous interventions across leading European centers, he joined the CUSL staff in 2020. Dr. Aphram specializes in adult cardiac surgery, with a focus on coronary bypass, valve repair, minimally invasive techniques, and robot-assisted mitral procedures. In 2025, he performed Belgium’s first robot-assisted aortic valve replacement, establishing CUSL as a leader in robotic cardiac surgery.
Background: Robotic mitral valve repair (RMVR) has gained significant recognition as minimally invasive alternative to conventional surgery, offering enhanced visualization, precision, minimize patient trauma and faster recovery. While early reports have shown encouraging outcomes, long-term data from high-volume centers remain limited. The aim of this study is to analyze perioperative and long-term clinical outcomes of patients undergoing robotic mitral valve repair at a single institution across a 12-year experience
Methods: This study includes all the patients who underwent RMVR in our institution between March 2012 and September 2024. Data were prospectively collected and retrospectively analyzed. Preoperative demographics, intraoperative characteristics, and postoperative outcomes were evaluated. Survival curves and freedom from reintervention were calculated using the Kaplan–Meier method.
Results: 336 patients were included in the study. Mean age was 58±12 years and 311 (92%) patients were male. Degenerative mitral valve disease was present in 98% of patients. All patients underwent successful mitral valve repair using different techniques, and 85 (25%) had one or more concomitant procedures. The mean cardio-pulmonary bypass and aortic cross clamp times were 155±36 and 106±26 minutes, respectively. There was no operative or in-hospital mortality. 6 patients (1.8%) required conversion to sternotomy. The need for a second cardiopulmonary bypass run was observed in19 patients (5.6 %). At discharge, 99% of patients had no or trivial residual regurgitation. Long-term follow-up confirmed durable repairs, with excellent survival and freedom from reintervention.
Conclusions: Our 12-year institutional experience confirms that robotic mitral valve repair is a safe and effective technique, even in complex pathologies. It provides durable long-term results with favorable outcomes, supporting RMVR as a standard approach in specialized centers.